Hormone Origins and Targets - MCAT Biological and Biochemical Foundations of Living Systems
Card 1 of 224
Which of the following is NOT a direct effect of the anterior pituitary?
Which of the following is NOT a direct effect of the anterior pituitary?
Tap to reveal answer
Milk production is influenced by prolactin (produced in the anterior pituitary). Bone growth is influenced by growth hormone (produced in the anterior pituitary). Ovulation is controlled by luteinizing hormone and follicle-stimulating hormone (both produced in the anterior pituitary). T4, a thyroid hormone, is controlled by thyroid-stimulating hormone (produced in the anterior pituitary). Water retention, on the other hand, is controlled by antidiuretic hormone (produced in the hypothalamus and released by the posterior pituitary).
Milk production is influenced by prolactin (produced in the anterior pituitary). Bone growth is influenced by growth hormone (produced in the anterior pituitary). Ovulation is controlled by luteinizing hormone and follicle-stimulating hormone (both produced in the anterior pituitary). T4, a thyroid hormone, is controlled by thyroid-stimulating hormone (produced in the anterior pituitary). Water retention, on the other hand, is controlled by antidiuretic hormone (produced in the hypothalamus and released by the posterior pituitary).
← Didn't Know|Knew It →
Scientists use a process called Flourescent In-Situ Hybridization, or FISH, to study genetic disorders in humans. FISH is a technique that uses spectrographic analysis to determine the presence or absence, as well as the relative abundance, of genetic material in human cells.
To use FISH, scientists apply fluorescently-labeled bits of DNA of a known color, called probes, to samples of test DNA. These probes anneal to the sample DNA, and scientists can read the colors that result using laboratory equipment. One common use of FISH is to determine the presence of extra DNA in conditions of aneuploidy, a state in which a human cell has an abnormal number of chromosomes. Chromosomes are collections of DNA, the totality of which makes up a cell’s genome. Another typical use is in the study of cancer cells, where scientists use FISH labels to ascertain if genes have moved inappropriately in a cell’s genome.
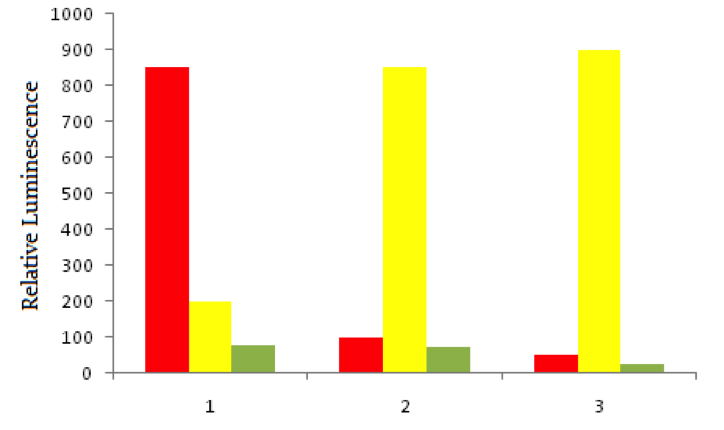
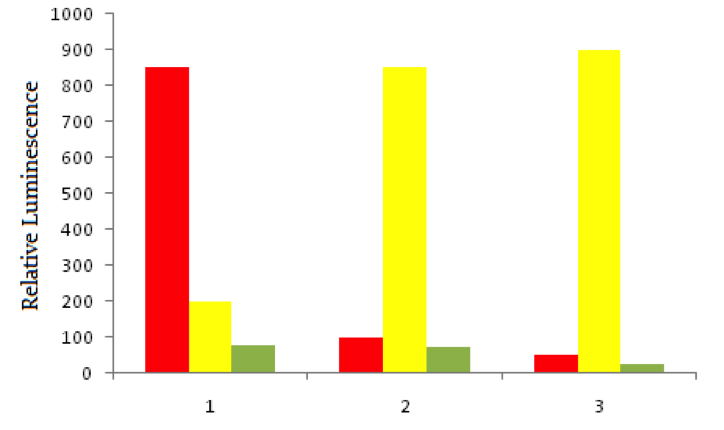
Using red fluorescent tags, scientists label probe DNA for a gene known to be expressed more heavily in cancer cells than normal cells. They then label a probe for an immediately adjacent DNA sequence with a green fluorescent tag. Both probes are then added to three dishes, shown below. In dish 1 human bladder cells are incubated with the probes, in dish 2 human epithelial cells are incubated, and in dish 3 known non-cancerous cells are used. The relative luminescence observed in regions of interest in all dishes is shown below.
Aneuploidy can also affect some fertilized zygotes after abnormalities in fertilization or gametogenesis. Aneuploid zygotes are typically spontaneously aborted before a pregnancy comes to term. A normal zygote binds to uterine endometrium while it is at its thickest, supported by progesterone secretion from which of the following?
Scientists use a process called Flourescent In-Situ Hybridization, or FISH, to study genetic disorders in humans. FISH is a technique that uses spectrographic analysis to determine the presence or absence, as well as the relative abundance, of genetic material in human cells.
To use FISH, scientists apply fluorescently-labeled bits of DNA of a known color, called probes, to samples of test DNA. These probes anneal to the sample DNA, and scientists can read the colors that result using laboratory equipment. One common use of FISH is to determine the presence of extra DNA in conditions of aneuploidy, a state in which a human cell has an abnormal number of chromosomes. Chromosomes are collections of DNA, the totality of which makes up a cell’s genome. Another typical use is in the study of cancer cells, where scientists use FISH labels to ascertain if genes have moved inappropriately in a cell’s genome.
Using red fluorescent tags, scientists label probe DNA for a gene known to be expressed more heavily in cancer cells than normal cells. They then label a probe for an immediately adjacent DNA sequence with a green fluorescent tag. Both probes are then added to three dishes, shown below. In dish 1 human bladder cells are incubated with the probes, in dish 2 human epithelial cells are incubated, and in dish 3 known non-cancerous cells are used. The relative luminescence observed in regions of interest in all dishes is shown below.
Aneuploidy can also affect some fertilized zygotes after abnormalities in fertilization or gametogenesis. Aneuploid zygotes are typically spontaneously aborted before a pregnancy comes to term. A normal zygote binds to uterine endometrium while it is at its thickest, supported by progesterone secretion from which of the following?
Tap to reveal answer
The corpus luteum forms after ovulation, when a pregnancy would be most expected. The corpus luteum secretes progesterone, which maintains the endometrium for potential implantation.
The corpus luteum forms after ovulation, when a pregnancy would be most expected. The corpus luteum secretes progesterone, which maintains the endometrium for potential implantation.
← Didn't Know|Knew It →
When calcitonin is released into the blood stream, the activity of which cell type is increased the most?
When calcitonin is released into the blood stream, the activity of which cell type is increased the most?
Tap to reveal answer
Calcitonin is a hormone secreted by the thyroid in response to increased blood calcium levels. It counteracts high blood calcium by stimulating the deposit of calcium into bone. Osteoblasts are the most active cells in building the hydroxyapatite matrix of bone, and would be most stimulated by the release of calcitonin.
Osteocytes are matured osteoblasts in the bond interior, and are more active in signaling and regulation than bond formation. Osteoclasts counteract osteoblasts and break down bone, usually in response to parathyroid hormone. Hydroxyapatite is the crystalline matrix encasing the bone cells, but is not a type of cell itself. Erythropoietic stem cells reside in the bone marrow and produce blood cells, but are not involved in calcium regulation.
Calcitonin is a hormone secreted by the thyroid in response to increased blood calcium levels. It counteracts high blood calcium by stimulating the deposit of calcium into bone. Osteoblasts are the most active cells in building the hydroxyapatite matrix of bone, and would be most stimulated by the release of calcitonin.
Osteocytes are matured osteoblasts in the bond interior, and are more active in signaling and regulation than bond formation. Osteoclasts counteract osteoblasts and break down bone, usually in response to parathyroid hormone. Hydroxyapatite is the crystalline matrix encasing the bone cells, but is not a type of cell itself. Erythropoietic stem cells reside in the bone marrow and produce blood cells, but are not involved in calcium regulation.
← Didn't Know|Knew It →
The activity of which of the following increases when parathyroid hormone is released into the blood stream?
The activity of which of the following increases when parathyroid hormone is released into the blood stream?
Tap to reveal answer
Parathyroid hormone causes calcium to be released from the bone into the blood stream, raising blood calcium levels. Osteoclasts reside in bone and are responsible for resorbing the hydroxyapatite matrix, releasing sequestered calcium into the blood.
Osteoblasts counter osteoclasts, building the hydroxyapatite matrix and sequestering calcium stores. Osteocytes are mostly involved in signaling. The parathyroid gland releases parathyroid hormone, but is not affected by the hormone itself. T-cell mature in the thyroid, and are not affected by parathyroid activity.
Parathyroid hormone causes calcium to be released from the bone into the blood stream, raising blood calcium levels. Osteoclasts reside in bone and are responsible for resorbing the hydroxyapatite matrix, releasing sequestered calcium into the blood.
Osteoblasts counter osteoclasts, building the hydroxyapatite matrix and sequestering calcium stores. Osteocytes are mostly involved in signaling. The parathyroid gland releases parathyroid hormone, but is not affected by the hormone itself. T-cell mature in the thyroid, and are not affected by parathyroid activity.
← Didn't Know|Knew It →
A person who has over-functioning pancreatic alpha cells may display what clinical feature?
A person who has over-functioning pancreatic alpha cells may display what clinical feature?
Tap to reveal answer
The pancreatic alpha cells produce the hormone glucagon, which is responsible for stimulating gluconeogenesis and glycogenolysis. Gluconeogenesis is de novo formation of glucose, while glycogenolysis is the breakdown of glycogen into glucose. An increase in glucagon production through hyperactive alpha cells will result in increased blood glucose levels, at least temporarily. In a healthy individual, this will be combatted by an increase in insulin production from the pancreatic beta cell.
The pancreatic alpha cells produce the hormone glucagon, which is responsible for stimulating gluconeogenesis and glycogenolysis. Gluconeogenesis is de novo formation of glucose, while glycogenolysis is the breakdown of glycogen into glucose. An increase in glucagon production through hyperactive alpha cells will result in increased blood glucose levels, at least temporarily. In a healthy individual, this will be combatted by an increase in insulin production from the pancreatic beta cell.
← Didn't Know|Knew It →
The hypothalamus uses two specialized types of neuron to stimulate the pituitary. Magnocellular neurons carry hormones directly to the posterior pituitary. Parvocellular neurons secrete hormones into the hypophyseal portal system, where they are delivered to the anterior pituitary.
The magnocellular neurons of the hypothalamus are responsible for secreting which hormone?
The hypothalamus uses two specialized types of neuron to stimulate the pituitary. Magnocellular neurons carry hormones directly to the posterior pituitary. Parvocellular neurons secrete hormones into the hypophyseal portal system, where they are delivered to the anterior pituitary.
The magnocellular neurons of the hypothalamus are responsible for secreting which hormone?
Tap to reveal answer
The hypothalamus is divided up into two parts: the magnocellular neurons and the parvocellular neurons. The magnocellular neurons synthesize antidiuretic hormone (ADH) and oxytocin, which are then transported to the posterior pituitary for secretion. The parvocellular neurons secrete hormones such as corticotropin-releasing hormone (CRH) and thyrotropin-releasing hormone (TRH), which are released into portal circulation to be transported to the anterior pituitary.
The hypothalamus is divided up into two parts: the magnocellular neurons and the parvocellular neurons. The magnocellular neurons synthesize antidiuretic hormone (ADH) and oxytocin, which are then transported to the posterior pituitary for secretion. The parvocellular neurons secrete hormones such as corticotropin-releasing hormone (CRH) and thyrotropin-releasing hormone (TRH), which are released into portal circulation to be transported to the anterior pituitary.
← Didn't Know|Knew It →
Glucose levels in the blood are maintained through the competing actions of two main hormones: insulin and glucagon. Other hormones like somatostatin, and catecholamines, such as acetylcholine, also serve to modulate glucose levels in the blood. Which molecule is produced by the beta cells of the islets of Langerhans in the pancreas?
Glucose levels in the blood are maintained through the competing actions of two main hormones: insulin and glucagon. Other hormones like somatostatin, and catecholamines, such as acetylcholine, also serve to modulate glucose levels in the blood. Which molecule is produced by the beta cells of the islets of Langerhans in the pancreas?
Tap to reveal answer
Beta cells in the islets of Langerhans are responsible for producing and secreting insulin in response to high blood glucose levels. In type I diabetes these cells are destroyed by an autoimmune process, while in type II diabetes they are replaced with scar tissue.
Alpha and delta cells in the islets of Langerhans produce glucagon and somatostatin, respectively. Neurons release acetylcholine to modulate glucose control through indirect processes.
Beta cells in the islets of Langerhans are responsible for producing and secreting insulin in response to high blood glucose levels. In type I diabetes these cells are destroyed by an autoimmune process, while in type II diabetes they are replaced with scar tissue.
Alpha and delta cells in the islets of Langerhans produce glucagon and somatostatin, respectively. Neurons release acetylcholine to modulate glucose control through indirect processes.
← Didn't Know|Knew It →
Glucose levels in the blood are maintained through the competing actions of two main hormones: insulin and glucagon. Other hormones, such as somatostatin, and catecholamines, such as acetylcholine, also serve to modulate glucose levels in the blood. Which molecule is produced by the alpha cells of the islets of Langerhans in the pancreas?
Glucose levels in the blood are maintained through the competing actions of two main hormones: insulin and glucagon. Other hormones, such as somatostatin, and catecholamines, such as acetylcholine, also serve to modulate glucose levels in the blood. Which molecule is produced by the alpha cells of the islets of Langerhans in the pancreas?
Tap to reveal answer
Alpha cells in the islets of Langerhans are responsible for producing and secreting glucagon in response to high blood glucose levels. Insulin antagonizes the alpha cells to prevent glucagon release. In diabetes, when the beta cells of the pancreas are not functional, extremely high levels of glucagon exist in the blood due to loss of the negative feedback loop.
Beta and delta cells in the islets of Langerhans produce insulin and somatostatin, respectively. Neurons release acetylcholine to modulate glucose control through indirect processes.
Alpha cells in the islets of Langerhans are responsible for producing and secreting glucagon in response to high blood glucose levels. Insulin antagonizes the alpha cells to prevent glucagon release. In diabetes, when the beta cells of the pancreas are not functional, extremely high levels of glucagon exist in the blood due to loss of the negative feedback loop.
Beta and delta cells in the islets of Langerhans produce insulin and somatostatin, respectively. Neurons release acetylcholine to modulate glucose control through indirect processes.
← Didn't Know|Knew It →
Type I diabetes is the result of an immune-mediated destruction of the beta cells in the islets of Langerhans in the pancreas. Which hormone would be expected to be elevated in type I diabetes?
Type I diabetes is the result of an immune-mediated destruction of the beta cells in the islets of Langerhans in the pancreas. Which hormone would be expected to be elevated in type I diabetes?
Tap to reveal answer
The first key to understanding this question is remembering that beta cells in the pancreas are responsible for secreting insulin. If the beta cells are destroyed, then insulin levels are low. Insulin and glucagon act in opposite ways to keep the concentration of blood glucose in the normal range, providing a negative feedback loop. Insulin inhibits glucagon, and glucagon inhibits insulin. If insulin is low, then glucagon will not be inhibited and will be produced at higher levels than normal.
The first key to understanding this question is remembering that beta cells in the pancreas are responsible for secreting insulin. If the beta cells are destroyed, then insulin levels are low. Insulin and glucagon act in opposite ways to keep the concentration of blood glucose in the normal range, providing a negative feedback loop. Insulin inhibits glucagon, and glucagon inhibits insulin. If insulin is low, then glucagon will not be inhibited and will be produced at higher levels than normal.
← Didn't Know|Knew It →
Type II diabetes results from prolonged overstimulation of the pancreatic beta cells as a result of obesity and chronically elevated glucose levels. After the beta cells have been overactive for an extended period of time, they begin functioning poorly and the person is considered diabetic. In a type II diabetes, what are the expected levels of insulin and glucagon with respect to normal values?
Type II diabetes results from prolonged overstimulation of the pancreatic beta cells as a result of obesity and chronically elevated glucose levels. After the beta cells have been overactive for an extended period of time, they begin functioning poorly and the person is considered diabetic. In a type II diabetes, what are the expected levels of insulin and glucagon with respect to normal values?
Tap to reveal answer
Type II diabetes results from an eventual lack of function of the pancreatic beta cells. The first step to this problem is remembering that the beta cells produce insulin. If the beta cells do not function, insulin levels will be decreased. The second step to this problem is remembering that insulin and glucagon have contrasting actions in the regulation of blood glucose levels. They act in a negative feedback loop: insulin inhibits glucagon release, and glucagon inhibits insulin release. If insulin levels are low, then glucagon will no longer be inhibited. As a result, we would observe low levels of insulin and elevated levels of glucagon.
Type II diabetes results from an eventual lack of function of the pancreatic beta cells. The first step to this problem is remembering that the beta cells produce insulin. If the beta cells do not function, insulin levels will be decreased. The second step to this problem is remembering that insulin and glucagon have contrasting actions in the regulation of blood glucose levels. They act in a negative feedback loop: insulin inhibits glucagon release, and glucagon inhibits insulin release. If insulin levels are low, then glucagon will no longer be inhibited. As a result, we would observe low levels of insulin and elevated levels of glucagon.
← Didn't Know|Knew It →
Which of the following hormones is least directly regulated by the anterior pituitary?
Which of the following hormones is least directly regulated by the anterior pituitary?
Tap to reveal answer
Epinephrine is released from the adrenal medulla and regulated by the sympathetic system.
Cortisone, progesterone, and thyroxin are regulated by adrenocorticotropic hormone (ACTH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH), respectively. These regulatory hormones are all released from the anterior pituitary. ACTH acts on the adrenal cortex to stimulate glucocorticoid release, including cortisone. LH acts on the ovaries to mediate estrogen and progesterone release. TSH acts on the thyroid to mediate the release of T3 and T4. T4 is also known as thyroxine.
Epinephrine is released from the adrenal medulla and regulated by the sympathetic system.
Cortisone, progesterone, and thyroxin are regulated by adrenocorticotropic hormone (ACTH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH), respectively. These regulatory hormones are all released from the anterior pituitary. ACTH acts on the adrenal cortex to stimulate glucocorticoid release, including cortisone. LH acts on the ovaries to mediate estrogen and progesterone release. TSH acts on the thyroid to mediate the release of T3 and T4. T4 is also known as thyroxine.
← Didn't Know|Knew It →
Which of the following statements concerning hormonal transport is true?
Which of the following statements concerning hormonal transport is true?
Tap to reveal answer
The type of transport that a hormone will have through the bloodstream depends on the type of hormone. Peptide hormones are polar and can move freely through the bloodstream, while lipid soluble hormones require a carrier protein in order to move through the blood. The pancreatic hormones, glucagon and insulin, are peptide hormones. This means they can move through the bloodstream without a carrier protein.
In contrast, steroid hormones are derived from cholesterol and thyroid hormones are derived from tyrosine. Both of these hormone classes are lipid soluble, and require transport proteins to travel through the blood. The hormone-protein unit is known as a chylomicron.
The type of transport that a hormone will have through the bloodstream depends on the type of hormone. Peptide hormones are polar and can move freely through the bloodstream, while lipid soluble hormones require a carrier protein in order to move through the blood. The pancreatic hormones, glucagon and insulin, are peptide hormones. This means they can move through the bloodstream without a carrier protein.
In contrast, steroid hormones are derived from cholesterol and thyroid hormones are derived from tyrosine. Both of these hormone classes are lipid soluble, and require transport proteins to travel through the blood. The hormone-protein unit is known as a chylomicron.
← Didn't Know|Knew It →
A male gymnast is suspected for using anabolic steroids (i.e. testosterone) to enhance in his athletic performance. Which of the following would you expect to be decreased in his blood?
A male gymnast is suspected for using anabolic steroids (i.e. testosterone) to enhance in his athletic performance. Which of the following would you expect to be decreased in his blood?
Tap to reveal answer
All three hormones—luteinizing hormone, follicle-stimulating hormone, and gonadotropin-releasing hormone—are part of the hypothalamic-pituitary-gonadal axis. One should be familiar with this axis and with the fact that testosterone exerts negative control at both the level of the hypothalamus and the anterior pituitary.
All three hormones—luteinizing hormone, follicle-stimulating hormone, and gonadotropin-releasing hormone—are part of the hypothalamic-pituitary-gonadal axis. One should be familiar with this axis and with the fact that testosterone exerts negative control at both the level of the hypothalamus and the anterior pituitary.
← Didn't Know|Knew It →
Which of the following hormones is not synthesized in the pituitary gland?
Which of the following hormones is not synthesized in the pituitary gland?
Tap to reveal answer
Oxytocin is the only hormone mentioned that is synthesized in the hypothalamus, but secreted by the posterior pituitary.
Oxytocin is the only hormone mentioned that is synthesized in the hypothalamus, but secreted by the posterior pituitary.
← Didn't Know|Knew It →
Which of these is NOT true of steroid hormones?
Which of these is NOT true of steroid hormones?
Tap to reveal answer
Because of their nonpolar nature, steroid hormones can easily cross the cell membrane. This enables the hormone to work with its receptor, commonly located inside the cell. Their effects are long-lived since they involve genetic alteration at the transcription level. This, however, also means that steroid hormones take longer than peptide hormones to produce a response.
Because of their nonpolar nature, steroid hormones can easily cross the cell membrane. This enables the hormone to work with its receptor, commonly located inside the cell. Their effects are long-lived since they involve genetic alteration at the transcription level. This, however, also means that steroid hormones take longer than peptide hormones to produce a response.
← Didn't Know|Knew It →
Which of the following is NOT one of the tropic hormones released by the anterior pituitary?
Which of the following is NOT one of the tropic hormones released by the anterior pituitary?
Tap to reveal answer
Prolactin is an example of a non-tropic hormone released by the anterior pituitary.
Prolactin is an example of a non-tropic hormone released by the anterior pituitary.
← Didn't Know|Knew It →
There are a large variety of over-the-counter pregnancy tests, although all of them share a set of common principles.
These home pregnancy tests are immunoassays which detect the presence of the peptide hormone human chorionic gonadotropin (hCG). hCG is produced by the fertilized ovum and released into the mother's bloodstream, preventing the degradation of the corpus luteum and thereby preventing menstruation. By the time of the mother's first missed period, hCG levels in the urine are high enough to detect.
The home pregnancy test generally involves dipping a stick containing immobilized hCG monoclonal antibodies into a urine sample. If hCG is present in the urine, it will bind to the monoclonal antibodies on the dipstick. The dipstick is then placed in a solution containing a second monoclonal antibody which recognizes the bound hCG antibody complex on the surface of the dipstick. This second antibody is conjugated to colloidal gold particles which change color when they are immobilized, indicating a positive test result (i.e., pregnancy).
The mechanism by which hCG acts on its target cells is most similar to that of .
There are a large variety of over-the-counter pregnancy tests, although all of them share a set of common principles.
These home pregnancy tests are immunoassays which detect the presence of the peptide hormone human chorionic gonadotropin (hCG). hCG is produced by the fertilized ovum and released into the mother's bloodstream, preventing the degradation of the corpus luteum and thereby preventing menstruation. By the time of the mother's first missed period, hCG levels in the urine are high enough to detect.
The home pregnancy test generally involves dipping a stick containing immobilized hCG monoclonal antibodies into a urine sample. If hCG is present in the urine, it will bind to the monoclonal antibodies on the dipstick. The dipstick is then placed in a solution containing a second monoclonal antibody which recognizes the bound hCG antibody complex on the surface of the dipstick. This second antibody is conjugated to colloidal gold particles which change color when they are immobilized, indicating a positive test result (i.e., pregnancy).
The mechanism by which hCG acts on its target cells is most similar to that of .
Tap to reveal answer
From the passage we learn that hCG is a peptide hormone. Peptide hormones act by binding to receptors on the plasma membranes of their target cells. This binding then triggers a signaling cascade which results in the transcription of specific genes. Peptide hormones can't cross the plasma membrane directly because they are not lipid soluble. Glucagon is a peptide hormone secreted by the alpha cells of the pancreas; it therefore uses a similar mechanism to that of hCG.The other answer choices can be eliminated because they are steroid hormones. These act by directly crossing the plasma membrane and binding to receptors either in the cytoplasm or in the nucleus.
From the passage we learn that hCG is a peptide hormone. Peptide hormones act by binding to receptors on the plasma membranes of their target cells. This binding then triggers a signaling cascade which results in the transcription of specific genes. Peptide hormones can't cross the plasma membrane directly because they are not lipid soluble. Glucagon is a peptide hormone secreted by the alpha cells of the pancreas; it therefore uses a similar mechanism to that of hCG.The other answer choices can be eliminated because they are steroid hormones. These act by directly crossing the plasma membrane and binding to receptors either in the cytoplasm or in the nucleus.
← Didn't Know|Knew It →
There are a large variety of over-the-counter pregnancy tests, although all of them share a set of common principles.
These home pregnancy tests are immunoassays which detect the presence of the peptide hormone human chorionic gonadotropin (hCG). hCG is produced by the fertilized ovum and released into the mother's bloodstream, preventing the degradation of the corpus luteum and thereby preventing menstruation. By the time of the mother's first missed period, hCG levels in the urine are high enough to detect.
The home pregnancy test generally involves dipping a stick containing immobilized hCG monoclonal antibodies into a urine sample. If hCG is present in the urine, it will bind to the monoclonal antibodies on the dipstick. The dipstick is then placed in a solution containing a second monoclonal antibody which recognizes the bound hCG antibody complex on the surface of the dipstick. This second antibody is conjugated to colloidal gold particles which change color when they are immobilized, indicating a positive test result (i.e., pregnancy).
Why isn't the presence of progesterone used as an indicator of pregnancy in the home pregnancy test?
There are a large variety of over-the-counter pregnancy tests, although all of them share a set of common principles.
These home pregnancy tests are immunoassays which detect the presence of the peptide hormone human chorionic gonadotropin (hCG). hCG is produced by the fertilized ovum and released into the mother's bloodstream, preventing the degradation of the corpus luteum and thereby preventing menstruation. By the time of the mother's first missed period, hCG levels in the urine are high enough to detect.
The home pregnancy test generally involves dipping a stick containing immobilized hCG monoclonal antibodies into a urine sample. If hCG is present in the urine, it will bind to the monoclonal antibodies on the dipstick. The dipstick is then placed in a solution containing a second monoclonal antibody which recognizes the bound hCG antibody complex on the surface of the dipstick. This second antibody is conjugated to colloidal gold particles which change color when they are immobilized, indicating a positive test result (i.e., pregnancy).
Why isn't the presence of progesterone used as an indicator of pregnancy in the home pregnancy test?
Tap to reveal answer
In order to be indicative of pregnancy, a hormone must only be produced either by a mother who is pregnant or the fertilized embryo itself. Otherwise, false test results might be possible. Progesterone is normally produced by females who are not pregnant during the course of their monthly menstrual cycles. It is not purely a hormone associated with pregnancy. The other answer choices do not offer valid explanations why progesterone can't be used.
In order to be indicative of pregnancy, a hormone must only be produced either by a mother who is pregnant or the fertilized embryo itself. Otherwise, false test results might be possible. Progesterone is normally produced by females who are not pregnant during the course of their monthly menstrual cycles. It is not purely a hormone associated with pregnancy. The other answer choices do not offer valid explanations why progesterone can't be used.
← Didn't Know|Knew It →
Both the sympathetic and the parasympathetic nervous systems are essential for homeostasis and for survival. For example, when we are trying to run away from a threat, the sympathetic nervous system is in full effect to allow us to escape from danger. However, when there is no obvious threat, the parasympathetic nervous system tends to be more in control.
There are similarities and differences between the sympathetic and the parasympathetic nervous systems. In preganglionic nerve fibers, both the sympathetic and the parasympathetic nervous system utilize the neurotransmitter acetylcholine. Closer to the target organ, the parasympathetic nervous system remains dependent on acetylcholine whereas norepinephrine and epinephrine are the predominant neurotransmitters utilized by the sympathetic nervous system.
When norepinephrine and epinephrine bind to their receptors, different effects are carried out based on the type of receptor, affinity, and location of the receptor. For example, epinephrine has a higher affinity for the beta-2 receptor. When epinephrine binds to the beta-2 receptor, common effects include vasodilation and bronchodilation. Norepinephrine has a stronger affinity for the alpha-1, alpha-2 and beta-1 receptors. When norepinephrine binds to its receptor, common effects on the body include vasoconstriction (alpha-1), increased heart rate (beta-1) and uterine contraction (alpha-1).
Patient A has a genetic disorder which prevents him from producing sufficient amount of catecholamines. Which of the following events will be affected in this patient.
I. Digestion
II. Pupil dilation
III. Erection
Both the sympathetic and the parasympathetic nervous systems are essential for homeostasis and for survival. For example, when we are trying to run away from a threat, the sympathetic nervous system is in full effect to allow us to escape from danger. However, when there is no obvious threat, the parasympathetic nervous system tends to be more in control.
There are similarities and differences between the sympathetic and the parasympathetic nervous systems. In preganglionic nerve fibers, both the sympathetic and the parasympathetic nervous system utilize the neurotransmitter acetylcholine. Closer to the target organ, the parasympathetic nervous system remains dependent on acetylcholine whereas norepinephrine and epinephrine are the predominant neurotransmitters utilized by the sympathetic nervous system.
When norepinephrine and epinephrine bind to their receptors, different effects are carried out based on the type of receptor, affinity, and location of the receptor. For example, epinephrine has a higher affinity for the beta-2 receptor. When epinephrine binds to the beta-2 receptor, common effects include vasodilation and bronchodilation. Norepinephrine has a stronger affinity for the alpha-1, alpha-2 and beta-1 receptors. When norepinephrine binds to its receptor, common effects on the body include vasoconstriction (alpha-1), increased heart rate (beta-1) and uterine contraction (alpha-1).
Patient A has a genetic disorder which prevents him from producing sufficient amount of catecholamines. Which of the following events will be affected in this patient.
I. Digestion
II. Pupil dilation
III. Erection
Tap to reveal answer
Catecholamines consist of epinephrine and norepinephrine. Without these neurotransmitter, the nervous system cannot illicit a sympathetic response. Of the answer choices, only pupil dilation is an event mediated by the sympathetic nervous system.
Catecholamines consist of epinephrine and norepinephrine. Without these neurotransmitter, the nervous system cannot illicit a sympathetic response. Of the answer choices, only pupil dilation is an event mediated by the sympathetic nervous system.
← Didn't Know|Knew It →
The brain is a very delicate structure with little room to move around. Surrounding the brain and the spinal cord are three protective layers in addition to the skull and the vertebral column. Directly surrounding the brain and spinal cord is the pia mater. Following the pia mater is the arachnoid mater. Between the pia mater and the arachnoid mater is the sub-arachnoid space where the cerebrospinal fluid circulates. Finally, the protective layer is the dura mater is loosely attached to the arachnoid mater but is strongly associated with the skull bone.
Depending on the type of injury, a certain type of vein and/or artery are more susceptible to injury. For example, the meningeal artery and vein run through the foramen spinosum and travel between the two layers making up the dura mater. As the artery and the vein are traveling in between the dura mater, there is a vulnerable region at the temple. A strike to the temple region could rupture these vessels and result in a epidural hematoma.
Traveling from the cerebral cortex to the venous dural sinus (located at certain regions between the two layers of the dura mater) is the cerebral vein. When an injury results in the dura mater shifting away from the arachnoid mater, the cerebral vein could rupture and lead to a subdural hematoma.
During a hematoma, the intercranial pressure could increase and push on certain regions of the brain. The compression of a certain region could either excite or inhibit the area. If patient A's laboratory results showed an increase blood concentration of antidiuretic hormone, which region of the brain is being compressed?
The brain is a very delicate structure with little room to move around. Surrounding the brain and the spinal cord are three protective layers in addition to the skull and the vertebral column. Directly surrounding the brain and spinal cord is the pia mater. Following the pia mater is the arachnoid mater. Between the pia mater and the arachnoid mater is the sub-arachnoid space where the cerebrospinal fluid circulates. Finally, the protective layer is the dura mater is loosely attached to the arachnoid mater but is strongly associated with the skull bone.
Depending on the type of injury, a certain type of vein and/or artery are more susceptible to injury. For example, the meningeal artery and vein run through the foramen spinosum and travel between the two layers making up the dura mater. As the artery and the vein are traveling in between the dura mater, there is a vulnerable region at the temple. A strike to the temple region could rupture these vessels and result in a epidural hematoma.
Traveling from the cerebral cortex to the venous dural sinus (located at certain regions between the two layers of the dura mater) is the cerebral vein. When an injury results in the dura mater shifting away from the arachnoid mater, the cerebral vein could rupture and lead to a subdural hematoma.
During a hematoma, the intercranial pressure could increase and push on certain regions of the brain. The compression of a certain region could either excite or inhibit the area. If patient A's laboratory results showed an increase blood concentration of antidiuretic hormone, which region of the brain is being compressed?
Tap to reveal answer
Antidiuretic hormone is produced by the hypothalamus and is released by the posterior pituitary. Therefore, compression either of these structures could provoke the release of antidiuretic hormone.
Antidiuretic hormone is produced by the hypothalamus and is released by the posterior pituitary. Therefore, compression either of these structures could provoke the release of antidiuretic hormone.
← Didn't Know|Knew It →